This post may contain affiliate links. Please read our disclosure policy.
Over the past few years, FODMAPs have gained notable attention as evidence continues to suggest reducing them can be a powerful way to resolve gut related issues. But, uh – what are FODMAPs? (And no, it’s not a new CrossFit workout.) Let’s explore.
Jump to:
What are FODMAPs?
FODMAP is a fancy little acronym that stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols.
The first word, fermentable, simply means what follows has the ability to ferment (specifically, in the gut.) The rest of the acronym are names of specific types of short-chain carbohydrates that aren’t completely digested in the small intestine.
While that may sound like a bad thing, short-chain carbohydrates that aren’t entirely absorbed are gobbled up and fermented by our resident gut flora, which keeps them fat and happy. Since our gut flora have a major influence on our overall health, including our ability to fight disease, these carbohydrates typically do the body good.[1][2]
But, for people with FODMAP intolerance – the game changes. Due to underlying issues, specific short-chain carbohydrates ferment in excess in both the small and large intestine, causing gas, bloating, and abdominal pain. These undigested carbohydrates also draw water into the large intestine, producing symptoms like bloat and diarrhea.[3]
Currently, a low-FODMAP diet has been shown to provide significant relief for some gut related issues, including the catch-all condition known as IBS (Irritable Bowl Syndrome.) In fact, studies show reducing FODMAPs has a 76% success rate for IBS sufferers.[4] Given that 1 in 5 people suffer from IBS, that’s kind of a big deal.
What Causes FODMAP Intolerance?
While researchers are still trying to figure out the underlying cause of FODMAP intolerance, there are some possible explanations. First, a condition know as SIBO (Small Intestinal Bacterial Overgrowth) has been closely connected with both FODMAP intolerance and IBS. SIBO is characterized by an overgrowth of pathogenic (bad) bacteria in the small intestine, which can feed on short-chain carbohydrates, causing excess fermentation (i.e. gas and bloating.)
So, in some cases, SIBO could be causing IBS and/or FODMAP intolerance; however, it’s also possible that FODMAP intolerance somehow contributes to SIBO. (Annnnd, yes, that’s a lot o’ acronyms.)
Given that the bacteria in our gut have a huge impact on our digestive health, it’s suspected other imbalances in gut flora (called dysbiosis) also contribute to FODMAP intolerance.
Other potential causes include intestinal permeability – also known as “leaky gut” which you can read about here, stress (which can cause leaky gut and inflammation), and lack of enzymes needed to appropriately digest short-chain carbohydrates.
Should I Reduce FODMAPs?
Since digestion is one big interconnected process, it’s hard to know for sure if your specific digestive issues will be resolved with a low-FODMAP diet. Other gastrointestinal disorders like SIBO or celiac disease should be ruled out first, which of course – you can do with the help of your doctor.
If you’re suffering from IBS or other functional gastrointestinal disorders – according to recent scientific literature, you have a pretty good chance of finding resolution.[5][6][7]
Also, if you’re suffering from chronic stress, reducing FODMAPs might help to alleviate common gastrointestinal symptoms. Stress not only changes the composition of our gut flora, it also inhibits the absorption of certain small-chain carbohydrates, causing excess fermentation.[8]
Given that a low-FODMAP diet ultimately reduces food sources for gut bacteria, it can also be helpful for those suffering from conditions like SIBO and dysbiosis. I know, I just told you to make sure you first “rule out” conditions like SIBO – but, there are many other treatment options that should be considered with your doctor.
It’s important to note, FODMAPs aren’t the underlying cause of digestive conditions such as IBS, they simply exacerbate symptoms. A low-FODMAP diet allows the gut to heal, and gives people an opportunity to figure out personal trigger foods.
How Do I Do This?
First off – you’ll be happy to know, a low-FODMAP diet isn’t something that should be implemented for life. Researchers suggest careful and intentional management of the diet as it can reduce or “alter” beneficial gut bacteria long-term.[9]
The Elimination Phase
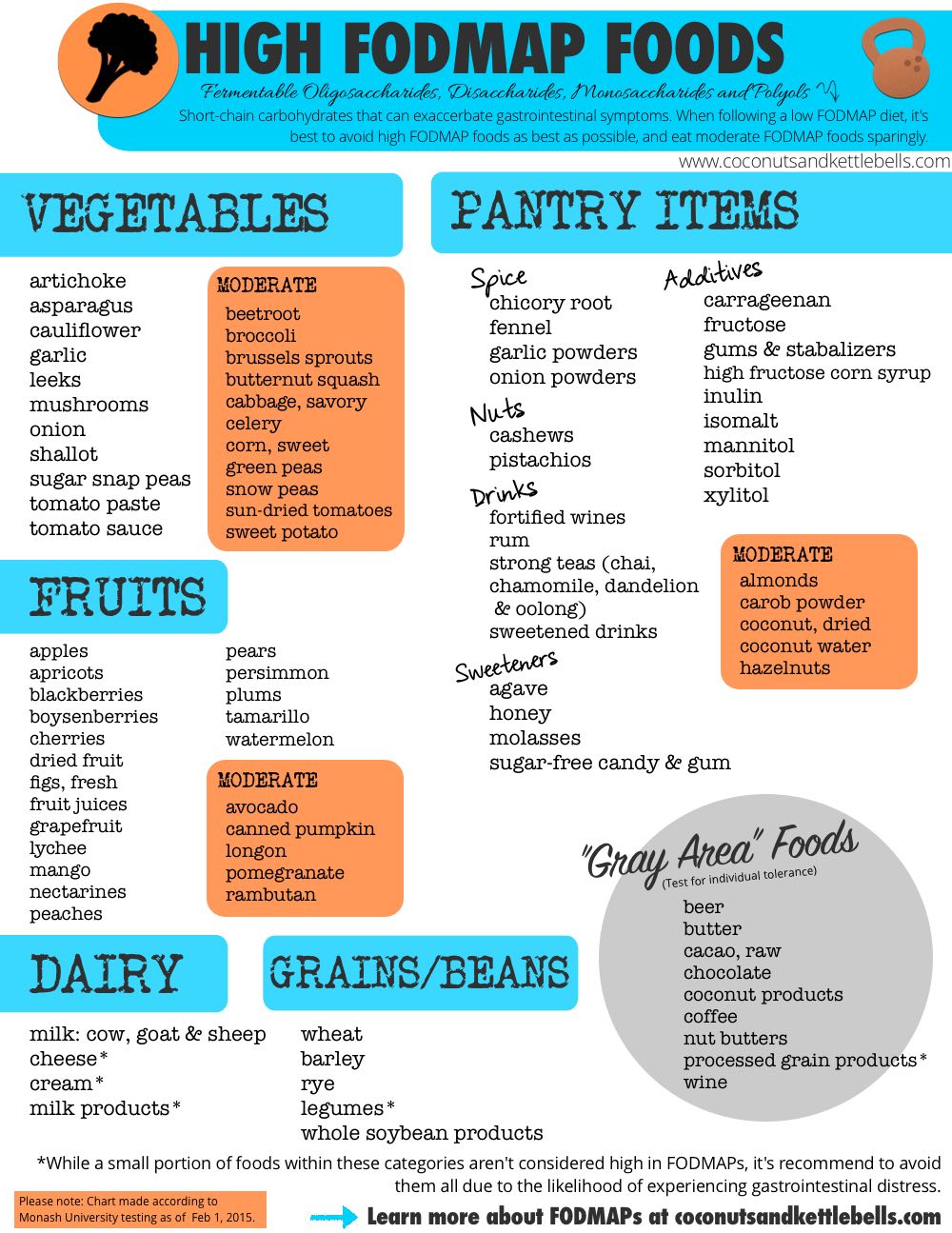
As a general recommendation, a low-FODMAP diet is an elimination diet that lasts for 6-8 weeks. During this time, high FODMAP foods are eliminated, and “moderate” FODMAP foods are reduced since some foods are dose dependent.
It’s also important to supplement with probiotics during this time.[10] Despite popular fermented foods like sauerkraut and milk kefir coming from high FODMAP food sources, slowly introducing fermented foods can be helpful for gut healing. Consider introducing coconut water kefir, or a tablespoon or two of sauerkraut juice during the elimination phase. (Helpful instructions on that can be found here.)
Throughout the elimination phase, it’s best to keep a notebook or word document that tracks what you ate and any changes in gastrointestinal symptoms. The objective is to stay in the elimination phase until the majority of symptoms have subsided. If no improvements occur, it’s important to work with your doctor to investigate other potential causes.
The Reintroduction Phase
After the elimination phase is complete, foods can be “challenged” in the reintroduction phase. Generally, you’ll want to stick with one FODMAP category at a time (polyols, for example), and choose foods that don’t contain multiple FODMAPs so you can isolate each category. Apples, for example, aren’t a good challenge food because they contain both polyols and fructose, which is a monosaccharide.
Because FODMAPs are dose dependent, it’s best to reintroduce foods in small amounts, and increase the dose over a few days – with a day or two in between to monitor symptoms. If no symptoms occur, you’ll move on to the next category. If symptoms occur, you’ll want to back off and allow your symptoms to subside before challenging a new food.
During the reintroduction phase, it’s important to remain on the low-FODMAP diet except for the challenge food, even if a food you’ve challenged did well. While it’s helpful to work with someone throughout this process, the template at the bottom of this document is a good place to start.
Wait. What are FODMAPs again?
So, there’s good and bad news. The bad news is – the list of high FODMAPs includes a lot of really tasty (and healthful) nutrient-dense foods. The good news is, this isn’t a long-term diet, and has the potential to make a big difference for those suffering from IBS symptoms.
And, the SUPER good news is – I’ve made a printable .pdf guide of the high and moderate FODMAP foods to make it easier on you! Download it here or click the image below, and it will automatically download.
Additional Guidance
During the elimination phase, you’ll want to avoid all high FODMAP foods as best as possible, and keep moderate FODMAP foods to 1/2 – 1 serving per meal. Keep in mind, moderate FODMAP foods are dose dependent. So, you may feel ok eating 1/8 of an avocado with other low-FODMAP foods, but feel distress when you combine it with 1/2 cup sweet potato. If you run into issues, use the guide above and your food journal to discover what might have caused your distress.
As an extra bonus, I’ve included “gray area foods” because there are some foods that are common sources of gastrointestinal distress. Some of these foods have tested low in FODMAPs, or haven’t been tested yet. As a general rule of thumb, it’s best to test these foods to figure out your personal tolerance, and be aware of how they affect you.
The printable guide above was created February 2015 using the most recent FODMAP testing information from Monash University. For the most up-to-date information on the exact FODMAP content of specific foods, you can download the Monasah University Low FODMAP App.
Have you found success on a low-FODMAP diet? I’d love to know your experiences below!
Live empowered,


Gay says
I want to use this diet to keep from getting SIBO again.
I do have one question for you regarding the FODMAP diet approach. I have food allergies and hist. Intol., so if I use the FODMAP diet, I don’t have much left to eat when I cut out broc, Cali, cabbage, asparagus , etc. etc.
Can eat eat small amounts of a.couple of these type foods at one meal or does the FODMAPS add up if I eat them all at once (even though I am eating them in the recommended quantities to be considered low FODMAP.)
Thanks for your time!
Noelle says
Hi Gay! As mentioned above, the FODMAP diet is not a long-term diet, and really should only be done for 6-weeks. During that period, you should cut out all high FODMAP foods, and forgo combining medium FODMAP foods. After six weeks, you reintroduce foods, and see which foods cause problems. Avoiding high FODMAP foods does NOT prevent SIBO. It only removes some of the foods that cause digestive distress when SIBO is present. Hope that helps!
G says
Thanks so much!
Paul says
Thanks for pulling together your excellent info graphic. Would love to know where you got the list of grey area foods. Whilst not traditional fodmap they are definitely problematic for me.
Noelle says
Yep! The grey area foods are “moderate” in FODMAPs or are known gut disruptors for some people, so they are largely depend on the person and the dose.
paul says
Thanks. Can u point me to any resources that discuss “gut disuptors” in more detail? I find vinegar also is abrasive to my guts. Would love to know more.
Noelle says
Hi Paul! This article is a great place to start!
Lexi says
Noelle,
I am struggling very very badly with fructose malabsorption (going on year two now) and I’m about at my wits end. It sucks to live like this- bloating to the point where I look pregnant as soon as I eat, so tired ALL THE TIME even if I get 9 hours of sleep and a sad, depressed attitude even though I know I’m not actually depressed.
I have had #allthetests but they haven’t shown anything. No SIBO or anything.
I went two days eating ONLY meat and healthy fats and felt 1000% better. As soon as I had one strawberry, BOOM. Bloated.
Do you have an recommendations for those who seem to be suffering from EXTREME fructose malabsorption? I’ve done strict low FODMAP for 5 months but it just isn’t enough. I am inclined to go no FODMAP but I am worried about that because I read “Sexy by Nature” and know how important carbohydrates are for a women’s body. But carbohydrates just seem to hate my intestines.
Any advice at all would be greatly appreciated.
Thank you, thank you!!
Lexi
Noelle says
Hi Lexi! So sorry you are struggling with this. I really think it would be worth it to work with a Functional Medicine Practitioner on this. Either online, or in person. I DO believe you can get past this. It might be a gut infection, or an imbalance of bacteria in the gut that is causing it. A specific, targeted approach to your condition is probably your best bet. Please let me know how it goes if you go this route!